Laboratory Studies
Platelet counts are elevated in a number of children with ADEM. Sedimentation rates are elevated in a third of patients. [47]
Modest-to-moderate elevation of CSF white and red blood cell counts may be found in childhood ADEM. Red blood cells may be due to modest degrees of AHLE. Elevated CSF HSV or Lyme titers do not exclude the possibility of associated ADEM, especially in recurrent herpes encephalitis. Results of CSF immune profile testing (eg, CSF:serum immunoglobulin G [IgG] index, CNS IgG synthetic rate, oligoclonality) employing age-appropriate normative data are positive in fewer than 10% of prepubertal children with ADEM. [10]
Positivity of studies for CSF oligoclonal bands and immunoglobulin elevation favors the diagnosis of MS in individuals younger than 20 years with first or recurrent bouts of acute CNS demyelinating illness. [7] In such instances it remains incumbent on those evaluating such individuals to exclude non-MS illnesses with specific biological markers such as systemic lupus, sarcoid, neuromyelitis optica, and so forth.
CSF myelin basic protein concentration level, reflecting demyelination, [83] is frequently elevated in ADEM.
Imaging Studies
The CT scan low-density abnormalities are found in more than half of childhood or adolescent ADEM cases, [47] but this technique is far less sensitive than MRI for the disclosure of extent and number of lesions.
T2-weighted and fluid attenuated inversion recovery (FLAIR), proton-density, or echo-planar trace diffusion MRI techniques disclose characteristic high-signal lesions in virtually all cases of ADEM. [47] T2/FLAIR images are particularly important in the evaluation of young individuals presenting with inflammatory CNS demyelinative illnesses that may be ADEM or MS. [11] Apparent diffusion coefficient maps show high-signal changes consistent with vasogenic edema.
ADEM lesions are characteristically multiple, bilateral but asymmetric, and widespread within the CNS.
-
Typical lesions of ADEM include centrifugal at the junction of the deep cortical gray and subcortical white matter. Such lesions are found in more than 90% of children with ADEM. They are found in less than 40% of adults initially diagnosed as having ADEM, many of whom are later diagnosed as having MS.
-
The indistinct margins of childhood ADEM lesions tend to suggest a "smudged" edge rather than the crisp margin typical of the classic ellipsoid plaques of MS.
-
Though variable, as many as 90% of childhood ADEM lesions enhance with gadolinium. The degree of contrast enhancement of ADEM lesions is typically uniform and usually not very dense. In contrast, MS plaques tend to vary in degree of contrast enhancement and may at times enhance quite densely. [12, 13, 14]
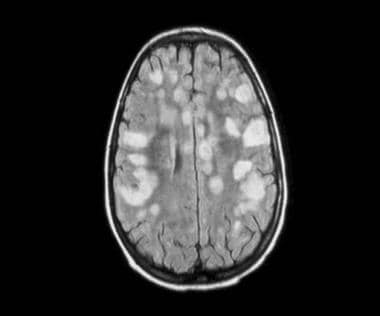
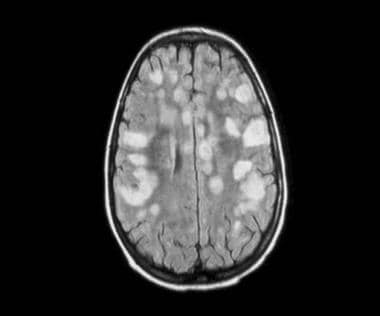 Typical childhood ADEM in 7-year-old. Note tendency to involve gray-white junction, the fact that the lesion margins are less well defined than typical MS plaques, and that the deep white matter lesions are not oriented perpendicularly to the ventricular surface as is typical in MS.
Typical childhood ADEM in 7-year-old. Note tendency to involve gray-white junction, the fact that the lesion margins are less well defined than typical MS plaques, and that the deep white matter lesions are not oriented perpendicularly to the ventricular surface as is typical in MS.
-
Many of the diseases that constitute the differential diagnosis of ADEM produce MRI abnormalities that emulate various ADEM-associated lesions.
Some cases of encephalitis result in the development of multiple tiny or small patches of bright signal on T2-weighted images that have been mislabeled as ADEM, but response to corticosteroid therapy is poor and follow-up scans may show severe encephalomalacia.
HSV-2 encephalitis or Lyme disease may be difficult to distinguish from ADEM and may involve ADEM mechanisms in pathogenesis.
Pial enhancement does not occur in ADEM and suggests meningoencephalitis.
Metazoal parasitic diseases of the brain (eg, cysticercosis), neoplasia, and ADEM are occasionally mistaken for one another.
Metabolic leukdystrophies may appear similar on MRI but often exhibit symmetric abnormalities in the white matter (as opposed to the asymmetric abnormalities seen in ADEM).
-
ADEM lesions may contain areas of hemorrhage suggestive of HSV-2 encephalitis, changes never found in MS plaques.
-
Unusual MRI abnormalities that are found in young individuals suspected of having ADEM may help greatly in distinguishing ADEM from MS or other alternative diagnoses. ADEM gives rise to a much wider variety of appearances than MS. ADEM may produce large unilateral T2 bright lesions, some of which appear to have striking central cavitation. These lesions may suggest neoplasm, stroke, parasitism, abscess, or MS. Ring enhancement or mass effect sometimes found in ADEM may suggest abscess or tumor. [15] In rare cases, symmetrical, linear, posteriorly emphasized white matter changes on T2 weighting suggest leukodystrophy. Recognize that no changes on MRI are pathognomonic of ADEM or, for that matter, of demyelination.
-
Some patients with ADEM have normal findings on MRI on initial presentation that become abnormal and characteristic of ADEM if the study is repeated several weeks later. [16] This suggests that characteristic features may be missed because of sampling error, that normal findings on a scan do not exclude the ADEM diagnosis, and that the appearance of new lesions during the course of ADEM may not represent recrudescence of disease.
Magnetization transfer MRI, single photon emission CT scanning, or nuclear magnetic resonance (NMR) spectroscopy may possibly prove helpful in distinguishing ADEM from alternative diagnoses, although the development of a pathognomonic imaging result is unlikely. For these reasons, diagnosing ADEM on the basis of findings on scanning alone is dangerous. Diagnosis of ADEM should always rest on clinical grounds in children as in adults.
-
Radiographic studies and other laboratory tests are especially valuable in ruling in or out alternative diagnoses.
From a retrospective analysis, Callen et al propose diagnostic criteria for MRI to distinguish a first MS attack in children from those with acute disseminated encephalomyelitis. Any 2 of the following criteria could distinguish MS from acute disseminated encephalomyelitis (sensitivity 81%, specificity 95%): (1) absence of a diffuse bilateral lesion pattern, (2) presence of black holes, and (3) presence of 2 or more periventricular lesions. [11]
Other Tests
See the list below:
-
The EEG often exhibits a disturbance of normal sleep rhythms and focal or generalized slowing. Epileptiform discharges are rarely seen in ADEM. [47] The absence of such abnormalities during the first bout of acute disseminated demyelinating illness in a child may increase the suspicion for ultimate MS diagnosis. Similar EEG abnormalities are found in adult ADEM. [84]
-
Visual evoked potentials (VEP) may prove helpful when optic neuritis is suspected but not apparent on clinical examination.
Procedures
The lumbar puncture is an essential aspect of acute disseminated encephalomyelitis (ADEM) workup. [17] It assists in distinguishing ADEM from various forms of meningoencephalitis, especially upon the basis of titers for the various bacteria, viruses, or other agents that may produce a directly infectious form of meningoencephalitis.
-
The immune profile is also helpful in distinguishing ADEM from MS. The IgG index, IgG synthetic rate, or oligoclonal bands are positive in more than two thirds of all first clinically recognized MS bouts and in 90-98% of individuals who have experienced multiple MS bouts. One or more of these studies is positive in a minority of ADEM cases.
-
Note that the findings on immune profile studies may be positive in various infectious conditions such as neurosyphilis, subacute sclerosing panencephalitis (SSPE), Lyme disease, stroke, and various forms of acute or chronic bacterial or viral meningoencephalitis. The CSF:serum IgG index or synthetic rate formulations may show positive results in neurosyphilis, Lyme disease, Guillain-Barré syndrome, some brain tumors, sarcoid, and a wide variety of bacterial or viral meningoencephalitides or other forms of CNS inflammation.
Occasionally, brain biopsy is necessary to distinguish ADEM from other diagnostic possibilities. The diagnosis of ADEM is confirmed when typical perivenular demyelinating changes with axonal sparing are observed. [47, 85]
-
Fatal case of ADEM involving the brainstem in a 13-month-old.
-
Typical childhood ADEM in 7-year-old. Note tendency to involve gray-white junction, the fact that the lesion margins are less well defined than typical MS plaques, and that the deep white matter lesions are not oriented perpendicularly to the ventricular surface as is typical in MS.
-
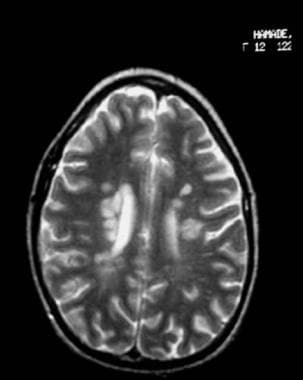
Typical adolescent multiple sclerosis findings on MRI. Note the tendency of lesions to exhibit sharp margins, to be elongated, to occur in deep white matter or corpus callosum sparing the cortical gray-white junction, and to be oriented perpendicularly to the ventricular surface.